Hyper-pigmentation is when patches of your skin changes colour. One cause for these discoloured areas could be medications or treatment you are taking for various ailments. Skin staining from drugs account for around 10-20% of hyperpigmentation or hypopigmentation and can cause emotional or psychological discomfort if these patches are noticeable by others.
Colour Derma understands that sometimes certain medications could cause physical side effects like skin hyper-pigmentation problems. We would like to do our part to inform you about the various causes of drug-induced skin staining so that you can get the support and assistance you need.
What treatments cause drug-induced skin staining?
Certain medications can affect your body in different ways. It could cause the accumulation of certain substances, such as iron, in skin layers causing a colour change. Or it could affect melanin levels in your body, creating darker or lighter patches of skin in different parts of your body. Here is a list of some of the treatments and the issues they may cause:
Heavy metals
If you have an iron deficiency, such as anaemia, you may get IV iron infusions. If some of that compound leaks out into your skin, it may accumulate enough to create brown patches. Gold was once a popular treatment for rheumatoid arthritis and could also cause brown discolouring. Silver salts is sometimes used for various medical and therapeutic purposes such as urethral irrigation, diabetes, and cancer. However, prolonged use may cause accumulations that create blue-grey patches to appear. Hyper-pigmentation issues caused by heavy metals may become permanent.

Minocycline
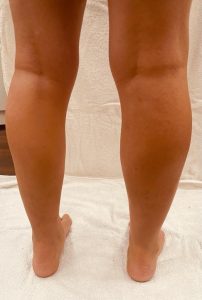
Minocycline is an antibiotic that is often used to treat acne as well as for various bacterial infections. Unfortunately, in higher doses, minocycline can cause a blue-black hyper-pigmentation around the arms and legs as well as around scarring and affected facial areas. Some colour changes could also occur in the fingernails. This has been known to occur among 2% to 15% patients studied. While it does fade over time, it has been known to take quite a while, sometimes years.
Antipsychotics
Doctors prescribe phenothiazines such as chlorpromazine for schizophrenia and manic depression. But they are also used to treat anxiety, chronic hiccups, nausea, and vomiting. Taking these drugs could cause an accumulative effect of blue or purple discolouring, especially in skin often exposed to the sun.
Amiodarone
Amiodarone is prescribed to treat serious irregular heartbeat conditions, or arrythmias. It is known to increase a patient’s sensitivity to the sun, and in some cases, it may cause blue-grey patches in those sun-exposed areas. These side-effects to wear away after the medication is stopped.
Anticonvulsants
People suffering from epilepsy may take phenytoin to control their seizures. Around 10% of them may develop round dark brown patches, which usually fade a few months after taking the medication.


Antimalarials
Those who take chloroquine or hydroxychloroquine for an extended period could, in about 25% of cases, find blue-grey patches on their faces, necks, and extremities. Exposed to the sun, they could turn to a darker blue-black.
Cytotoxic treatments
Several cancer drugs, such as busulfan for leukemia, bleomycin for lymphoma and ovarian and other cancers, doxorubicin for various cancers, and Cyclophosphamide, which is also used for autoimmune conditions, all have been known to cause discolouration of some type.
Cortisone
Cortisone injections are often an effective treatment for arthritis and other joint conditions. Among about 4% of patients develop discolouration around the injection site which can be quite noticeable, especially among darker toned people who experience lighter patches appearing. Depending on the person and length of treatment, this may become permanent.


NSAIDs
Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can sometimes cause a fixed drug eruption. This is like an allergic reaction when the skin reacts with a scar-like discolouration appearing.
Other treatments
While this may seem like a long list, it is by no means exhaustive. There are other drugs and treatments that have known side effects which include skin hyper-pigmentation problems. So, we at Colour Derma strongly recommend that you discuss these possible side effects with your medical professional, or, if unusually discolourations appear, make sure to disclose all the medications you are taking to ensure proper diagnosis.
Will the discolouration go away?
As discussed above, different drugs have different effects that are not always permanent. Discussing this with your healthcare provider is key. It may be as simple as stopping the medication, lowering dosages, or switching to a different treatment.
There may also be other things you can to do reduce the skin staining. Mainly, you can protect your skin from valtrex sun exposure as it may enhance the discoloured areas. Apply sunscreen with the highest SPF you can, cover up with hats or long sleeves and trousers, or avoid going out in direct sunlight as much as possible.
Camouflage make-up is another option. Whether the effect is permanent, or you are waiting for the discoloured patches to fade, camouflage cosmetics can conceal the affected areas. This is especially beneficial if those patches are on your face, hands, or other exposed areas and are making your self-conscious. Properly applied, camouflage make-up can give you a natural look so you can go out with confidence.

Talk to Colour Derma about camouflage makeup
The team at Colour Derma are experts in camouflage makeup, and we all have vast experience helping people regain their confidence as they deal with their skin condition, including drug-induced hyper-pigmentation issues. We offer products for a wide range of camouflage makeup options to suit various needs. Contact Colour Derma today to discuss which solution is best for you.


Recent Comments